

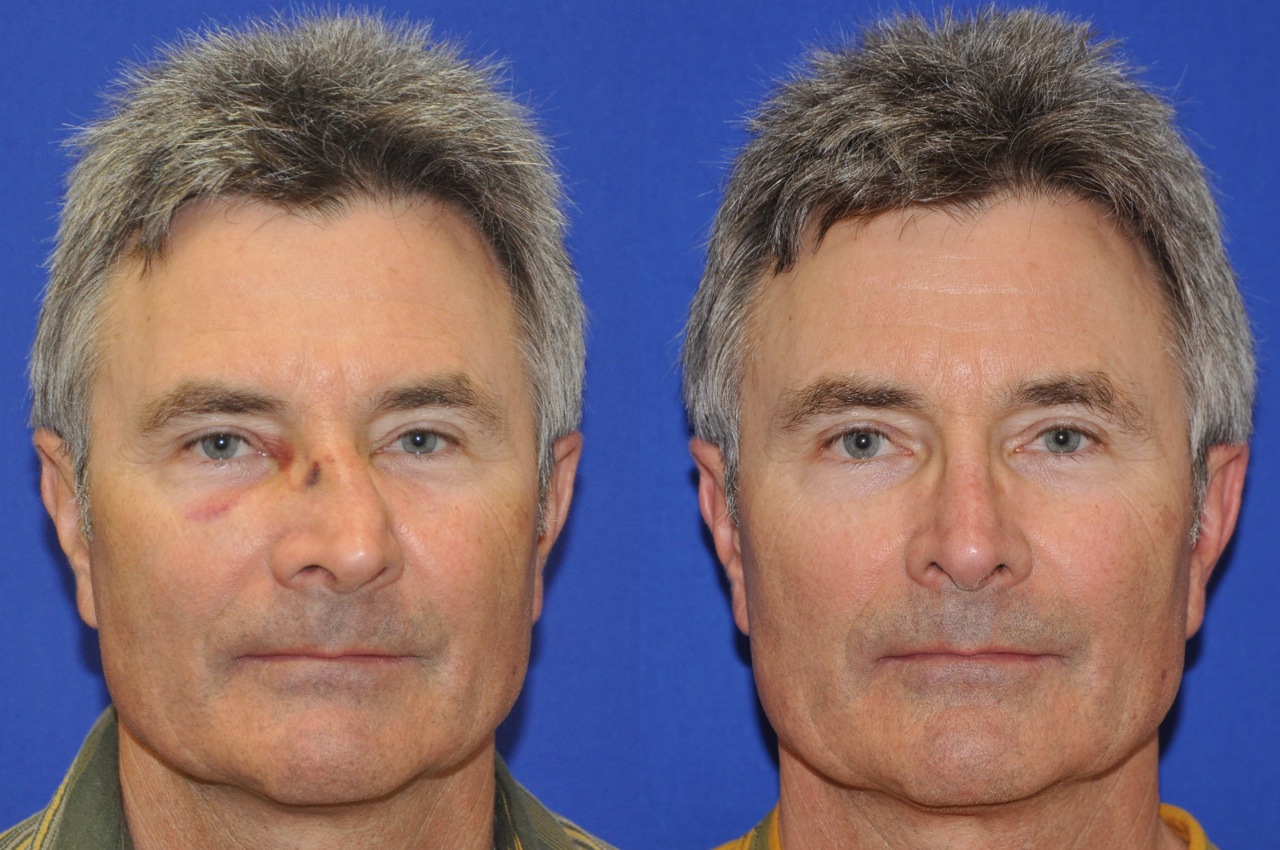
- #A patient underwent closed reduction of a closed fracture skin#
- #A patient underwent closed reduction of a closed fracture full#
19 Nonoperative treatment for displaced scapular neck fractures > 10 mm demonstrated only 15.7% patient satisfaction, versus 94.7% satisfaction with displacement < 10 mm. 16–18Ī 2018 systematic review of all scapular fracture types reported satisfactory results in 90.4% (N = 629) of nonoperatively treated patients and 93.7% (N = 512) of operatively treated patients. Consideration for ORIF should be made in cases involving glenohumeral instability, intra-articular involvement, and displacement. In both groups, nonoperative management consists of sling immobilization with progression to physical therapy at two weeks. Although traditionally considered high energy injuries (e.g. automobile accident), low energy injuries may occur in the elderly. Scapula fractures can be divided based on the energy (i.e., amount of force causing the fracture) involved and fracture location.
Weight bearing 12 weeks for neck or body fracture
#A patient underwent closed reduction of a closed fracture full#
Partial to full weight bearing as tolerated Weight bearing when tolerated Two-Six weeksįemur fractures, proximal and shaft, should not be treated nonoperatively ROM active / resistance exercises four weeks ROM active / Resistance exercises six weeks Switch to above elbow cast when comfortable One-Two weeks passive ROM, active ROM Four-Six weeks when painless Two-Three weeks gentle ROM or active assisted six weeks active resistanceĭC brace when active abduction painless and no fracture movementĭistal humerus, olecranon, coronoid, radial headĩ0-degree post mold cast or sling One-Two weeks Although these fracture patterns may initially be treated by an emergency medicine physician or other primary care provider, in the United States, these fractures are, as a standard of care, referred for fracture management to an orthopedic surgeon. Due to subjective nature of considering closed fracture management options, it is recommended that each case be taken individually and tailored to the patient’s particular fracture pattern and morphology. 10 Tables Tables1 1 and and2 2 depict the modes of immobilization, when to start range of motion, and when to return to normal function based on medical textbooks 11,12 as well as the senior authors’ (i.e., BB, DW, RV) clinical experiences. Immobilization treatments of closed fractures (e.g., slings, splints, casts traction avoidance of weight bearing) are still the most widely used method of fracture management. 8 During the 1930s, the addition of binders (e.g., starches, gums, and dextrins) made commercial bandage preparation more feasible, although it wasn’t until the mid-1940s that commercial plaster bandages became commonly used. In 1852, the Dutch military surgeon Matthysen devised a method to coat and infuse cotton bandages with gypsum to make the first casting bandages.

6,7 The use of plaster was first described in 1798 by British surgeons who had observed Persians using gypsum. 3 Bandages with lime and egg white have also been recorded by Arabic physicians.

5Įarly methods to stabilize fractures recorded by Hippocrates included linen splints stiffened with gum and plaster bandages suffused with resins, gums, and waxes. Although lay bonesetters have not been accepted by many mainstream medical communities, 4 present-day bonesetters in developing nations may still have their services preferred over modern medical techniques. 3 In developing nations, “bonesetters” in Asia, Africa, and in native populations of North and South America have typically been non-medically trained practitioners treating fractures and reducing joint dislocations with skills developed using an apprentice model. 3 He noted the five following principles of care: antisepsis, reduction, traction, bandaging, and splinting. 2Īt approximately 400 b.c., Hippocrates wrote three books “Fractures,” “Articulations, and”Instruments of Reduction” for fracture management. 1 Egypt was also the site of the earliest examples of active fracture care (e.g., splints) on an unhealed femur fracture, dated around 300 b.c. 1 The earliest documentation of fracture care was in the Egyptian “Edwin Smith” papyrus, circa 1600 b.c.
#A patient underwent closed reduction of a closed fracture skin#
Through the 20th century, the nonsurgical treatment of closed fractures (i.e., when bone is broken, but skin intact) have been the standard of care.


 0 kommentar(er)
0 kommentar(er)
